Herd Immunity Is Not the Primary Goal of Vaccination
Monday, April 5, 2021
Indonesian Technical Advisory Group on Immunization (ITAGI) Chair Sri Rezeki Hadinegoro said that the Covid-19 immunization has been fairly smooth albeit the vaccine shortage. The high mortality rate among the elderly population has prompted the government to shuffle the order of priority groups for vaccination. On the advice of the ITAGI, the elderly group was moved forward from the fourth to the second in line to be vaccinated along with public servants. Accoding to Sri Rezeki the main objective of vaccination was not to create heard immunity as widely publicized but rather to lower the death rate. Not only participating in the preparation of vaccination roadmap, the ITAGI also gives recommendations to the health ministry.
arsip tempo : 174395148264.
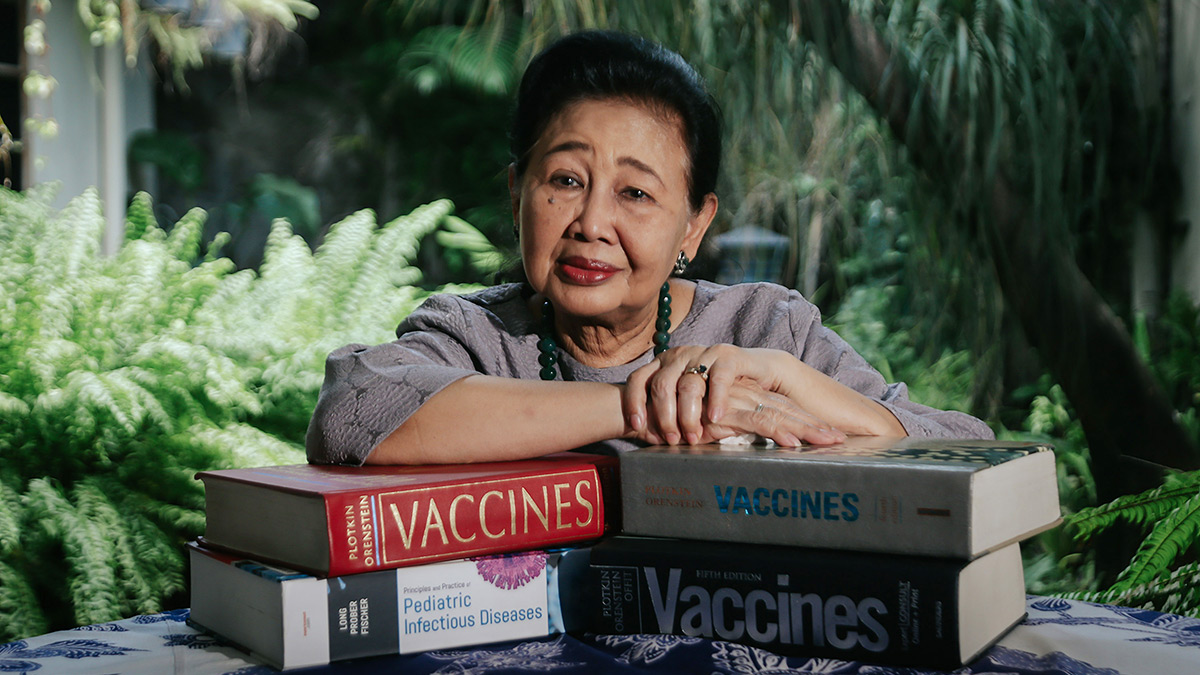
THE high mortality rate from Covid-19 among the elderly population has spurred the government to re-orientate its vaccination policy. On the recommendation of the Indonesian Technical Advisory Group on Immunization (ITAGI), the health ministry included older people in the second phase of the vaccination program. People above 60 years old previously slated to be vaccinated in the fourth round were injected with vaccine alongside public servants on
...
Subscribe to continue reading.
We craft news with stories.
 For the benefits of subscribing to Digital Tempo, See More
For the benefits of subscribing to Digital Tempo, See More